The New Era of Digital Dentistry
The field of dentistry is undergoing a profound transformation driven by 3D printing technology. Moving from traditional plaster models and manual fabrication to today’s highly efficient and precise digital workflows, 3D printing has become a critical tool for modern clinics seeking to enhance efficiency and patient experience. Although currently only 17% of US dentists use 3D printers in clinical practice, 67% of these users have been operating them for less than two years, indicating that the technology is in an early growth phase.
This article aims to provide a comprehensive guide to selecting dental 3D printing resins, covering material properties, clinical applications, and market trends, helping you make informed investment decisions.
The Standardized Workflow of Dental 3D Printing
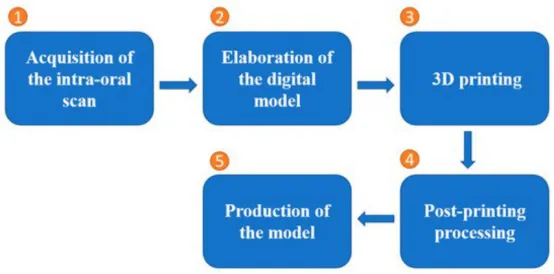
The success of modern dental 3D printing relies on a standardized, closed-loop digital workflow, which ensures a seamless transition from data acquisition to final product:
- Acquisition of the intra-oral scan: Obtaining digital data of the patient’s mouth using an intra-oral scanner (data acquisition).
- Elaboration of the digital model (CAD Design): Designing and optimizing the data using CAD software (CAD design).
- 3D Printing: Transforming the digital model into a physical entity using a 3D printer.
- Post-printing processing: Crucial steps including cleaning (with alcohol or solvents) and curing (with UV light).
- Production of the model: Finalizing the end product, such as a diagnostic model or surgical guide.
Clinical Benefits and Challenges to Adoption
The benefits brought by digital 3D printing technology to clinics are significant:
- Improved Efficiency and Cost Reduction: 68% of users report improved efficiency, and 44% have achieved cost reduction. 3D printing can also lower costs by reducing reliance on external lab outsourcing for tasks like surgical guide production.
- Diverse Applications: The most common applications include diagnostic models, surgical guides, splints, and occlusal devices.
- Support for Personalized Treatment: The technology supports personalized treatments and minimally invasive surgeries, such as the precise creation of implant guides.
However, challenges remain for broader adoption, primarily focusing on: material long-term stability, biosafety verification, equipment cost, and the need for manual intervention during post-processing steps. Nevertheless, 21% of non-users plan to invest in 3D printing in the future, and 35% are considering relevant training.
Selecting the Right Resin: Properties, Applications, and Limitations
Choosing the appropriate resin is the foundation of successful 3D printing. Different clinical needs require different resin characteristics.
1. Dental Model Resins
| Key Property | Typical Value/Description | Clinical Applicability | Limitation |
|---|---|---|---|
| Accuracy & Stability | Viscosity 150–350 mPa·s, low shrinkage | Orthodontic aligner design, removable prosthodontic and orthodontic models, supports restoration fitting | Limited to non-biocontact applications |
| Hardness | Shore Hardness 80–85 D | Smooth surface | Post-processing requires shrinkage control for assembly accuracy |
2. Temporary Crown and Bridge Resins
These resins are used to create temporary restorations, offering the advantages of quick production and lower cost.
- Biocompatibility Requirements: Evaluation must follow standards like GB/T 16886.1 and YY/T 0268.
- Primary Risk: Residual monomers (e.g., methacrylate-based materials) may cause delayed allergic reactions (e.g., mucositis), particularly in the fresh state, though toxicity decreases after polymerization.
- Mitigation Strategy: It is recommended to reduce oral contact through indirect manufacturing (using a dental model) and strictly adhere to post-curing procedures.
3. Surgical Guide Resins
Surgical guides are essential for implant procedures, and their accuracy directly impacts implantation success.
- Accuracy Factors: Material selection and post-curing are crucial. Resins like GC’s LS resin and NextDent™ SG resin have shown the highest transfer accuracy.
- Mechanical Characteristics: Low Young’s Modulus resins may improve accuracy, suitable for distal free-end guides.
- Sterilization Requirements: Classified as high-risk devices, high-pressure steam or plasma sterilization is recommended, as these methods do not affect hardness, strength, or volume.
4. Splint/Nightguard Resins
Used for occlusal protection devices, requiring high mechanical strength to withstand long-term masticatory forces.
- Mechanical Performance Standards: Ultimate flexural strength should be ≥ 50 MPa, and flexural modulus of elasticity ≥ 1500 MPa. For instance, ISO 4049 requires flexural strength ≥ 80 MPa and compressive strength ≥ 250 MPa for long-term durability.
- Comparative Advantage: 3D printed resins (P group) and CAD/CAM PMMA blocks (M group) often show higher flexural strength compared to self-curing acrylic resins (SC group).
- Limitation: Surface roughness needs optimization through polishing.
5. Castable Resins
Used to create wax patterns for casting crowns and bridges, ultimately supporting the production of metal or ceramic restorations.
- Core Challenge: The burnout process requires strict control over the temperature curve. For example, staged heating to 732°C (held for 180 minutes), followed by slow cooling to the casting temperature (e.g., 482°C).
- Risk: Improper handling during the burnout process can lead to model cracking or dimensional distortion.
Resin Selection Guide by Clinic Type
Different clinic types should prioritize specific resins based on their core business and application frequency.
| Clinic Type | Recommended Resin Categories | Key Decision Factors | Certification & Safety Requirements |
|---|---|---|---|
| General Dental Clinics | Dental Model Resins (for diagnostic models), Temporary Crown/Bridge Resins (for quick repairs) | Turnaround time, staff skill (post-processing training), equipment compatibility (DLP/LCD systems) | Focus on biocompatibility for temporary crown/bridge resins |
| Orthodontic Clinics | Dental Model Resins (for clear aligner models), Splint Resins (for nightguards) | Resin must be compatible with orthodontic appliances, low cytotoxicity photopolymerization resins are preferred | ISO 10993 cytotoxicity certification |
| Restorative Labs | Castable Resins (for metal framework), High-Precision Model Resins | Burnout process control, bio-certification (e.g., FDA approval) to ensure restoration safety | FDA approval, ISO biosafety benchmarks |
| Oral Surgery Centers | Surgical Guide Resins , Gingival Mask Resins | Guide accuracy directly impacts surgical success, standardized sterilization procedures (steam sterilization), DICOM data compatibility | High-precision requirement , compliance with sterilization protocols |
Emerging Trends and Future Outlook
The dental 3D printing market is forecasted to reach $7.9 billion by 2027, with material innovation being a crucial driver of growth.
- Hybrid and Nanofilled Resins: Nanofillers can significantly enhance the resin’s mechanical strength and dimensional stability.
- Biocompatible and FDA-Approved Materials: The trend is towards materials with low cytotoxicity. It is essential to select materials approved through FDA (510(k)/PMA) or ADA science affairs committee processes.
- Digital Workflow Integration: Open data standards like DICOM promote interoperability between devices. Systems like DTX Studio™ integrate the entire process from imaging to restoration, further enhancing precision and efficiency.
Conclusion and Expert Recommendation
A successful investment in dental 3D printing is a comprehensive consideration, not just about equipment cost. Clinics should prioritize:
- Clinical Need and Accuracy: Select resins that meet the required viscosity, hardness, and shrinkage standards for the specific application (e.g., models, guides).
- Biosafety and Certification: ISO 10993 and FDA/ADA certified biocompatible materials must be chosen, especially for restorations with long-term patient contact.
- Workflow and Cost-Efficiency: Evaluate the complexity of the required post-processing steps (cleaning, curing, polishing), and ensure equipment-resin compatibility. By internalizing high-turnover applications (like model printing), initial equipment investment can be effectively distributed, achieving long-term cost savings.
By making targeted resin choices and standardizing operating procedures, your clinic will be able to fully leverage the potential of 3D printing, optimize treatment outcomes, and ultimately stay ahead in the era of digital dentistry.

