What Is a Gingival Mask and Why Does It Matter?
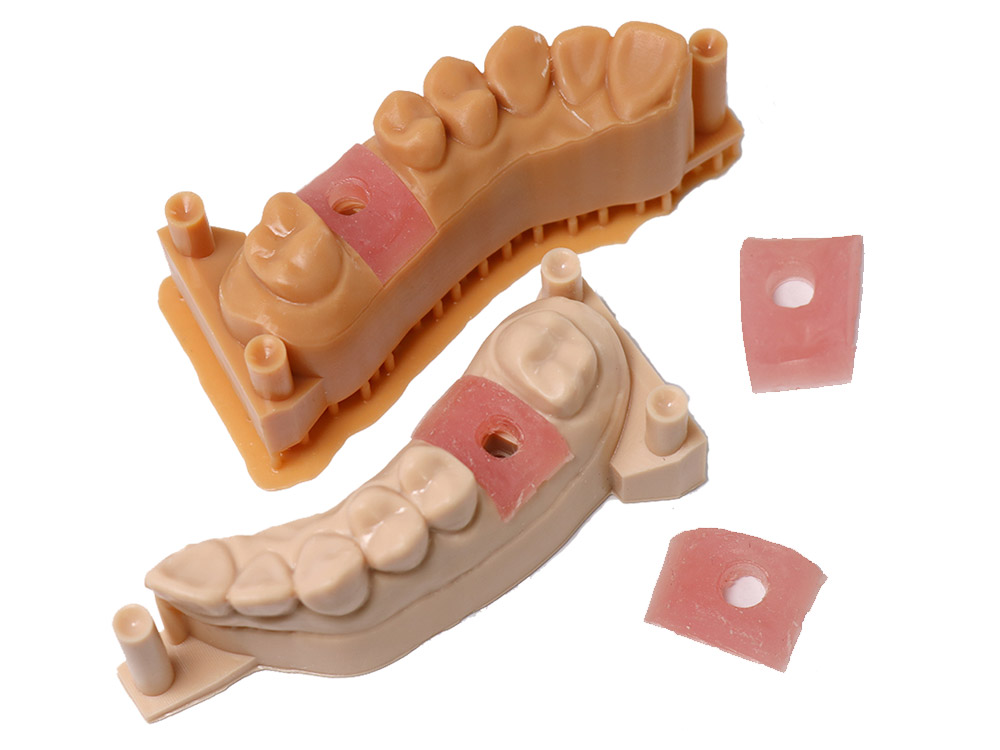
A gingival mask is a 3D-printed soft tissue simulation that recreates a patient’s gum contours with remarkable accuracy. Unlike traditional hard tissue models that only show bone structure, the gingival mask provides a complete oral environment by adding realistic, flexible gum tissue over the bone model.
In implant dentistry, this technology bridges a critical gap. While digital planning software can show bone density and anatomy, it often overlooks how soft tissues will interact with implants and surgical guides. The gingival mask solves this problem by providing a physical representation of the patient’s actual gum thickness, contours, and tissue characteristics.

How the Gingival Mask Is Created: From Digital Scan to Physical Model
The process begins with comprehensive digital data collection. Dentists use intraoral scanners to capture detailed soft tissue topography, while CBCT imaging provides the underlying bone structure. Advanced dental CAD software then segments and models the gingival tissues separately from the hard tissues.
The magic happens during printing. Using specialized flexible resins, 3D printers create a gingival mask that feels and behaves like real gum tissue. The mask is then overlaid onto a traditional hard tissue model, creating a complete oral simulation that includes both bone and soft tissue components.
The result is a patient-specific model that allows dentists to visualize, test, and plan procedures in a realistic environment before touching the actual patient.
Three Critical Advantages of the Gingival Mask in Clinical Practice
1. Enhanced Visual Planning Prevents Aesthetic Complications
The Clinical Challenge: Dr. Rodriguez encountered a challenging case involving a 34-year-old photographer who needed an anterior implant. Using traditional planning methods with only hard tissue models and radiographs, the treatment seemed straightforward. However, during surgery, the gingival tissue proved much thicker than anticipated, requiring immediate adjustments to implant positioning.
How the Gingival Mask Solves This: With gingival mask technology, Dr. Rodriguez could have seen the exact tissue thickness and contour variations before surgery. The flexible mask material accurately represents gingival thickness, biotype, and natural contours, allowing precise visualization of how the implant will interact with surrounding tissues.
Clinical Outcome: In subsequent cases using the gingival mask, Dr. Rodriguez achieved predictable aesthetic results. The mask revealed tissue thickness variations as small as 0.5mm, enabling optimal implant positioning that preserved natural gingival architecture and achieved excellent emergence profiles.
Key Benefits:
- Accurate assessment of gingival biotype (thick vs. thin)
- Precise visualization of tissue contours and thickness
- Better prediction of post-surgical tissue behavior
- Reduced risk of aesthetic complications
2. Improved Surgical Guide Accuracy Eliminates Intraoperative Problems
The Clinical Challenge: Dr. Kim was placing multiple posterior implants in a 58-year-old patient using a carefully designed surgical guide. Despite meticulous digital planning, the guide wouldn’t seat properly during surgery due to interference from thick gingival tissues that weren’t accounted for in the planning phase.
How the Gingival Mask Solves This: The gingival mask allows pre-surgical testing of guide fit and function. The flexible tissue simulation shows exactly where soft tissue interference might occur, enabling guide modifications before the actual procedure. Dentists can perform complete mock surgeries on the gingival mask model, identifying and resolving potential issues.
Mock Surgery Benefits: Dr. Kim now tests all surgical guides on gingival mask models before surgery. During one recent case, the mock surgery revealed that the guide design would compress tissue and cause blanching. The team modified the guide design, removing material from tissue-contact areas and adding relief channels.
Clinical Outcome: The revised surgical guide seated perfectly during the actual procedure, with all four implants placed in precise positions within 20 minutes. The patient experienced minimal discomfort due to optimized tissue management.
Key Benefits:
- Pre-surgical guide testing and validation
- Identification of soft tissue interference points
- Opportunity for guide design modifications
- Reduced surgical time and complications
3. Superior Patient Communication and Treatment Acceptance
The Clinical Challenge: Dr. Thompson struggled to help a 65-year-old retired teacher understand her complex full-arch treatment plan. Despite detailed explanations and digital presentations, the patient remained anxious about the extensive procedure and concerned about the final appearance.
How the Gingival Mask Solves This: Physical models with realistic gum tissue provide tangible, understandable representations of treatment plans. Patients can hold and examine the models, seeing exactly how their gums will look after healing. The realistic tissue simulation helps patients visualize outcomes in ways that digital images cannot achieve.
The Consultation Experience: Using a gingival mask model, Dr. Thompson demonstrated the entire treatment process. The patient could see how implants would integrate with her existing gum tissue and how the final restorations would emerge naturally. The physical model answered questions that words and images couldn’t address.
Clinical Outcome: The patient immediately gained confidence in the treatment plan and scheduled her procedure. She later reported that the physical model “made everything clear” and eliminated her fears about the outcome.
Key Benefits:
- Tangible visualization of treatment outcomes
- Enhanced patient understanding and confidence
- Improved treatment acceptance rates
- Reduced patient anxiety and concerns
Essential Properties of an Effective Gingival Mask
Realistic Tissue Simulation
An effective gingival mask must replicate the feel and behavior of natural gum tissue. The ideal material provides sufficient flexibility to allow compression and manipulation while maintaining dimensional stability. This balance enables accurate testing of surgical procedures and guide placement.
Dimensional Accuracy
Precision is crucial for the gingival mask to be clinically useful. A high-quality mask maintains dimensional accuracy within 0.1mm or better, ensuring that surgical guides designed using the model will fit perfectly in the patient’s mouth.
Biocompatibility and Safety
Since the gingival mask may be used during patient consultations, the material must be biocompatible and safe for human contact. Non-toxic, low-odor materials ensure comfortable patient interactions during treatment planning discussions.
Durability and Chemical Resistance
A clinical gingival mask must withstand repeated handling, disinfection, and sterilization procedures. Chemical resistance to common dental disinfectants allows safe reuse while maintaining accuracy and appearance.
Clinical Applications: Where the Gingival Mask Makes the Biggest Impact
Aesthetic Zone Implant Planning
In the anterior region, the gingival mask is invaluable for assessing papilla preservation, emergence profile optimization, and tissue thickness evaluation. It helps predict post-surgical tissue behavior and guides implant positioning for optimal aesthetic outcomes.
Complex Multi-Implant Cases
Full-arch reconstructions and multiple implant placements benefit significantly from gingival mask technology. The mask enables comprehensive mock surgeries, guide testing, and prosthetic planning in a realistic soft tissue environment.
Guided Bone Regeneration Procedures
When combining implant placement with bone grafting, the gingival mask helps plan flap design, membrane placement, and tissue management strategies. The realistic tissue simulation guides surgical approach and helps predict healing outcomes.
Revision and Corrective Procedures
Failed implant cases and soft tissue deficiencies require careful planning. The gingival mask helps visualize current tissue conditions and plan reconstruction approaches, including soft tissue grafting and implant repositioning.
Integration into Digital Workflows
Planning Phase
The gingival mask integrates seamlessly with existing digital planning workflows. After completing virtual planning, teams create physical models that include both hard and soft tissue components for comprehensive evaluation.
Pre-Surgical Preparation
Mock surgeries on gingival mask models allow teams to practice complex procedures, test instrument access, and identify potential complications before treating patients.
Patient Education
Physical models serve as powerful educational tools, helping patients understand their conditions and proposed treatments more clearly than digital presentations alone.
The Future of Soft Tissue Simulation in Dentistry
Gingival mask technology represents a significant advancement in predictable implant dentistry. As 3D printing materials and techniques continue to improve, we can expect even more realistic tissue simulations that further enhance treatment planning and patient outcomes.
The integration of soft tissue simulation into routine implant planning protocols is becoming standard practice in leading dental offices. This technology doesn’t just improve clinical outcomes—it transforms the entire patient experience by providing clarity, confidence, and predictability.
Conclusion: Transforming Implant Dentistry Through Realistic Simulation
The gingival mask bridges the gap between digital planning and clinical reality. By providing accurate soft tissue simulation, it enables dentists to visualize, test, and refine treatment plans before surgery begins. This technology reduces complications, improves outcomes, and enhances patient satisfaction.
As implant dentistry continues to evolve toward greater precision and predictability, the gingival mask is becoming an essential tool for practices committed to excellence. The ability to see, touch, and test treatment plans in a realistic environment represents a fundamental shift toward more successful, patient-centered care.
The future of implant dentistry lies in comprehensive simulation that includes all aspects of the oral environment. The gingival mask is leading this transformation, making complex procedures more predictable and successful for both dentists and patients.

