TAMPA, FLORIDA – Groundbreaking research into dry eye disease, led by Dr. Yuqiang Bai from the University of South Florida (USF) Morsani College of Medicine’s Ophthalmology department, is making significant strides thanks to innovative 3D printing technology. The research, funded by a prestigious National Institute of Health (NIH) grant, aims to better understand and image dry eye disease by measuring the thickness of tears on the cornea.
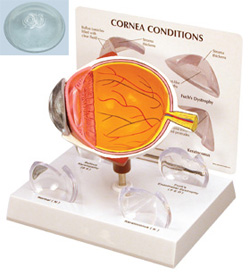
Dry eye disease affects millions globally, causing discomfort and vision problems. To study this condition accurately, Dr. Bai’s team needs to precisely image the curved surface of the cornea. However, traditional imaging systems typically use flat standards, such as the 1951 USAF resolution test chart, which are unsuitable for the cornea’s unique curvature.
To overcome this challenge, the 3D Print Lab at USF IT, led by Lucas Tometich, has played a crucial role. They have employed advanced 3D modeling and printing techniques to create a model that accurately mimics the curvature of the cornea.
Tometich explained, “Based on the requirements provided, I created a model using Autodesk Fusion. We conducted several tests to determine the optimal orientation and post-processing workflow, ensuring we achieve the clearest results with clear photopolymer resin. We have made a few adjustments this week and delivered three more pieces for testing with the scanner.”
The Role of 3D Printing in Dry Eye Research
The primary principle and mechanism of applying 3D printing in dry eye disease research lie in creating highly accurate physical models with specific shapes and curvatures to simulate the surface of the human cornea. This enables researchers to overcome the limitations of traditional imaging methods when dealing with curved biological tissues.
- Precise Geometric Replication: 3D printing technology can accurately reproduce physical objects with curvatures similar to the human cornea based on digital models. This is crucial for testing and calibrating devices that need to interact with or precisely measure the corneal surface.
- Serving as a Standard Test Object: The printed corneal models can serve as standardized test objects for evaluating and optimizing the performance of novel imaging systems (such as Dr. Bai’s team’s laser scanner). By testing on models with known curvatures, researchers can ensure the imaging system accurately measures tear film thickness and other key parameters.
- Simulating Real Physiological Conditions: While current 3D printed models primarily simulate geometry, future developments may include integrating microfluidic channels or other structures to more realistically mimic tear distribution and dynamics.
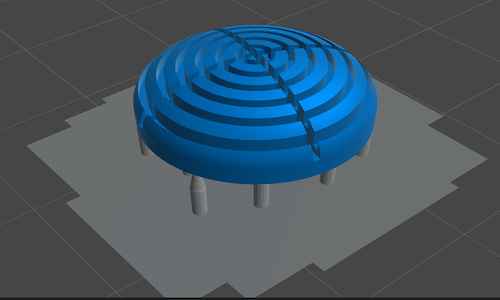

In short, 3D printing facilitates the development and validation of more accurate and reliable diagnostic and research tools for dry eye disease by providing a physical reference with precise corneal curvature, thereby advancing the in-depth understanding of the disease and the development of novel therapies.
This collaboration highlights the vital role of information technology in advancing medical research. By providing a standard sample that accurately represents the cornea’s curvature, 3D printing enables Dr. Bai’s team to move forward with the development of their imaging system. This system is expected to provide more detailed information about dry eye disease, potentially leading to the development of more effective treatments and improved patient outcomes.
Dr. Bai emphasized the model’s critical importance, stating, “We needed a model that mimics the curvature of the cornea’s surface to demonstrate the feasibility of our imaging system. Until we had one, we weren’t able to proceed with our research.”
The 3D Print Lab is part of the University of South Florida’s IT Advanced Visualization Center (AVC). The AVC is dedicated to supporting students, faculty, and researchers with advanced technologies by providing development, training, and implementation for courses and research projects.